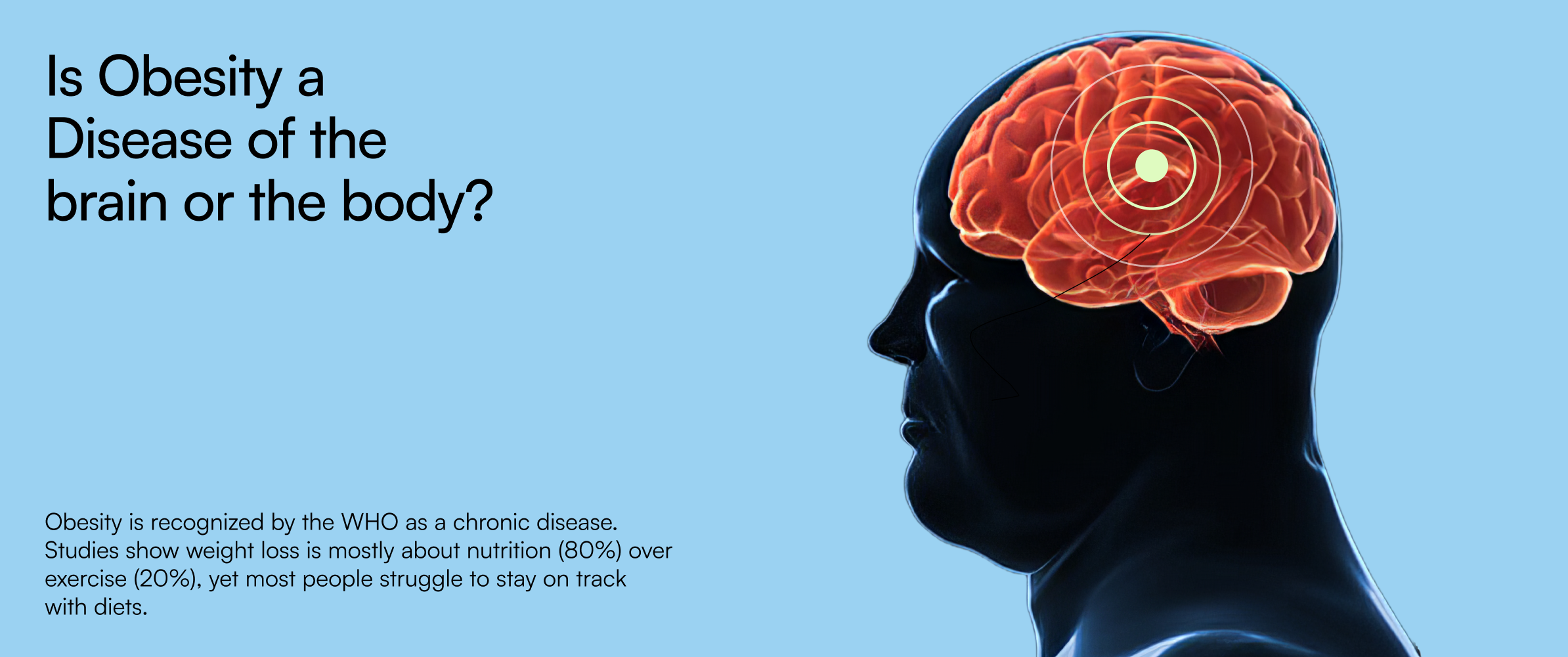
Is Obesity a Disease of the brain or the body?
Dr. Krishna Prabhakar, Internal Medicine and Critical Care specialist, explains how brain circuits, hormones, genetics, and metabolism interact in obesity, and why modern, evidence-based care works far better than willpower-driven weight loss approaches.

Understanding Obesity: More Than Just Weight Gain
Before answering whether obesity is driven by the brain or the body, it is important to clarify what is obesity.
The medical obesity meaning goes far beyond excess body weight. Obesity is a chronic, relapsing metabolic disease characterized by abnormal or excessive fat accumulation that increases the risk of long-term health complications. It affects how the brain regulates hunger, how hormones signal fullness, and how the body stores and burns energy.
This is why obesity behaves differently from person to person and why a single diet or workout plan rarely works for everyone.
“Why Do I Regain Weight the Moment I Stop Dieting?”
This is one of the most common questions I hear in clinical practice.
Despite calorie restriction, clean eating, or intense exercise routines, many people experience rapid weight regain. This pattern is not caused by poor discipline. It reflects the underlying causes of obesity, rooted in altered biology.
Today, nearly one in three adults lives with obesity, and many also carry silent metabolic risks such as pre-diabetes, type 2 diabetes, high blood pressure, fatty liver disease, and cholesterol abnormalities.
At its core, obesity represents a continuous tug-of-war between the brain’s appetite and reward pathways and the body’s metabolic systems. When these systems are dysregulated, weight regain becomes almost inevitable.
Common Obesity Symptoms People Often Ignore
Many individuals do not recognize early obesity symptoms, especially when weight gain occurs gradually. These symptoms often include:
- Persistent hunger or cravings despite eating balanced meals
- Difficulty losing weight even with consistent effort
- Low energy levels and poor stamina
- Sleep disturbances or daytime fatigue
- Increased stress-related or emotional eating
- Gradual development of insulin resistance or metabolic syndrome
These are not personal shortcomings. They are biological signals indicating deeper metabolic dysfunction.
The Daily Reality: Living With Obesity
If any of the following experiences sound familiar, you are not alone:
- Persistent cravings despite “eating clean” all week
- Repeated weight cycling after diets, detoxes, or fitness programs
- Low energy levels even after seven to eight hours of sleep
- Stress eating after long workdays or emotional exhaustion
- Weight loss plateaus despite regular walking or gym workouts
These patterns reflect the reasons for obesity that go beyond food choices alone, including hormonal adaptation, stress physiology, and neurochemical changes in the brain.
Is Obesity Controlled by the Brain or the Body?
The answer is not either-or. It is both.
Obesity is a brain–body disease.
The brain determines hunger, fullness, cravings, and food reward through complex neural circuits. The body, through organs such as the gut, liver, muscle, and fat tissue, executes these signals using hormones like insulin, leptin, ghrelin, and GLP-1.
When these systems are disrupted, the body actively defends its weight. This explains why dieting often leads to stronger hunger signals, slower metabolism, and eventual weight regain.
Understanding what is obesity at this level helps explain why treating calories alone rarely leads to lasting results.
The Real Causes and Reasons for Obesity
The causes of obesity are multifactorial and interconnected. They include:
- Genetic predisposition affecting appetite and fat storage
- Hormonal imbalances involving insulin, leptin, and ghrelin
- Altered gut-brain signaling and reward pathways
- Chronic stress, poor sleep, and inflammation
- Long-term metabolic adaptation after repeated dieting
These reasons for obesity explain why obesity persists even in individuals who are motivated, educated, and health-conscious.
A Major Shift in How We Treat Obesity
Over the last decade, obesity treatment has evolved significantly.
We now treat obesity as a chronic disease, similar to diabetes, hypertension, or heart disease. Modern care focuses on correcting underlying biology first, then supporting lifestyle changes that become sustainable rather than exhausting.
One of the most important advances has been the use of GLP-1 receptor agonists, medications that mimic natural gut-brain hormones involved in appetite regulation.
GLP-1 medications help by:
- Increasing satiety and reducing hunger
- Calming food cravings and emotional eating
- Improving insulin sensitivity and blood sugar control
- Supporting gradual, sustainable weight loss
When combined with protein-focused nutrition, strength training, and optimized sleep and stress management, patients experience meaningful and lasting improvements.
Why Lifestyle Changes Alone Often Fail
Nutrition and exercise are essential, but they are not always sufficient.
In individuals with long-standing obesity, insulin resistance, or metabolic syndrome, lifestyle changes alone often trigger stronger hunger signals and reduced energy expenditure. This biological pushback explains why so many people experience frustration and burnout.
Medical support does not replace lifestyle changes. It makes them achievable by addressing the root causes of obesity.
The ReverseAll Medical Weight Management Protocol
At ReverseAll, obesity care is never reduced to a prescription alone.
Our integrated approach treats both the brain and body, offering personalized, evidence-based care.
The ReverseAll protocol includes:
- Clinician-led medical assessment
Comprehensive metabolic testing, medication review, and screening for type 2 diabetes, PCOS, fatty liver disease, and hypertension - Guided GLP-1 therapy
Eligibility evaluation, individualized dosing, side-effect management, and structured discontinuation planning - Nutrition and strength training support
A protein-first dietary approach, fiber targets, electrolyte balance, and resistance training to preserve lean muscle mass - Behavioral and lifestyle coaching
Practical strategies for improving sleep quality, managing stress, and controlling cravings - Ongoing follow-ups and progress tracking
Regular reviews, data-driven adjustments, and long-term support
What Patients Commonly Experience With Comprehensive Care
Patients receiving structured medical weight management often report:
- Clinically significant weight loss and reduced waist circumference, a key marker of visceral fat
- Improved blood sugar levels, including lower fasting glucose and HbA1c
- Better blood pressure control, healthier cholesterol levels, and improved fatty liver markers
- Higher energy levels and improved overall quality of life
- Better adherence because hunger and cravings become manageable
Individual results vary, but addressing both obesity symptoms and underlying biology improves long-term outcomes.
So, Is Obesity a Disease of the Brain or the Body?
The answer is clear: both.
Obesity is a brain–body condition. The brain sets the appetite and energy regulation signals, while the body executes them through hormones, metabolism, and tissue function. Treating one without the other leads to short-term success and long-term disappointment.
Treating brain signaling and body metabolism together is modern, compassionate, and effective care.
If you are exploring medical weight loss options or feeling exhausted by repeated plateaus, it may be time to rethink what is obesity and how it should be treated.
At ReverseAll, we combine medical expertise, nutrition, and personalized coaching so your weight loss plan fits your biology and your life.